
Melasma: Everything You Need to Know
There is no easy way to deal with discoloured skin. Facial discolouration is even worse because there isn’t much that you can do to hide it. This is how melasma manifests. About 6 million Americans and many more millions of people globally are dealing with this.
A condition previous associated with pregnant women and referred to as the “mask of pregnancy” affects other women as well and 1 man in every 20 women. So, how much is known about melasma? We have compiled everything you need to know about melasma below.
What is Melasma?
Melasma is a form of skin hyperpigmentation that manifests as blotchy, dark patches on the forehead, cheeks and sometimes on the chin and jawline. It is also referred to as chloasma or the ‘mask of pregnancy’ when it occurs in pregnant women. The irregular patches may be brown, tan greyish or blue-grey depending on your complexion.

Melasma occurs when cells become hyperactive, causing overproduction of melanin in certain parts of the skin. This is the same mechanism that leads to ages spots and freckles but melasma patches tend to be larger and more stubborn to treat.
Who is Likely to Get Melasma?
Anybody can get melasma. However, it is rare in men and may only affect about 10% of them. It is also less common in puberty and post-menopausal periods. People with darker skin type are more likely to get melasma compared to their fair-skinned counterparts. This is probably due to the fact that darker skin naturally has more pigment-producing cells.
In a summary, the following people are at a greater risk of getting melasma:
- Women of reproductive age (30-55 years)
- People of Hispanic, Asian and African descent
- Individuals with a family history of the condition
- People who live in areas with high-intensity ultraviolet radiation (UVR)
What causes Melasma?
Melasma has different causes. However, all cases of melasma can be linked back to three main factors; hormonal change, racial/familial predisposition and exposure to sunlight.
Hormonal changes
Hormones are closely linked to melasma. That is why many cases of melasma are reported in pregnant women, women on hormonal birth control and menopausal women on Hormone Replacement Therapy (HRT).
When a woman is pregnant, her body increases the production of oestrogen, progesterone, and melanocyte stimulating hormones. This is especially so during the third trimester. This can trigger the onset of melasma.
Interestingly, progesterone is believed to be more closely tied to cases of melasma compared to oestrogen. How so? Women on birth control pills containing progesterone or menopausal women given progesterone for HTR have been reported to display more cases of melasma.
This could be the reason why fewer males get melasma; because they produce progesterone too. However, their levels are not exposed to erratic fluctuations compared to women.

Racial/familial Predisposition
If melasma runs in your family, you might just be in line to get it as well. In a study involving 324 patients in various centres, 48% had family histories of melasma. While there have not been any studies to associate genes with melasma, quite a significant number of studies have shown credible association between familial/racial predisposition and cases of melasma.
UV light Exposure
Exposure to UV light cannot cause melasma on its own. However, when the background of predisposition and hormonal changes is already set, it plays the greatest role in triggering and advancing the condition. This stems from the ability of chronic sun exposure to cause overproduction of melanin.
What is the Impact of Melasma on you?
Melasma does not pose any health risks to you or cause any pain.
Dark patches are the worst you can expect, there should be no other signs or symptoms. On the other hand, the dark patches and their facial position can be a source of emotional distress for anyone suffering from melasma. This can reduce self-esteem and may significantly affect your social life.
Can Melasma Go Away on its Own?
Given the various causes of melasma, it can go away on its own. This can be greatly determined by the underlying causes. Sometimes, pregnancy-related melasma can resolve on its own after one gives birth. The same may happen when one stops taking birth control pills or HRT. Unfortunately, there is no way to determine when that is likely to happen. This is where one seeks different ways to treat the discolouration.
Should Melasma Be Treated During Pregnancy
Melasma usually gets worse during pregnancy because of the live triggers. It is therefore even harder to treat. For this reason, it is pointless to try and treat it and better to wait until the delivery of the baby.
How to Diagnose and Treat Melasma
Treating melasma starts with a dermatologist’s confirmation of the condition and determination of the underlying cause. Treating the hyperpigmentation without addressing the underlying cause will not bear any fruit if triggers are still active.
To diagnose melasma, a dermatologist physically examines your skin. For an even better look into how deeply it penetrates your skin, he/she may use a device known as a Wood’s light.
Sometimes, melasma can look like other conditions. To rule out other conditions, the dermatologist may do a skin biopsy. This involves removing and testing a small bit of skin. The procedure is safe and fast enough to be done at a dermatology office. Skin biopsy is a rare requirement most of the time.
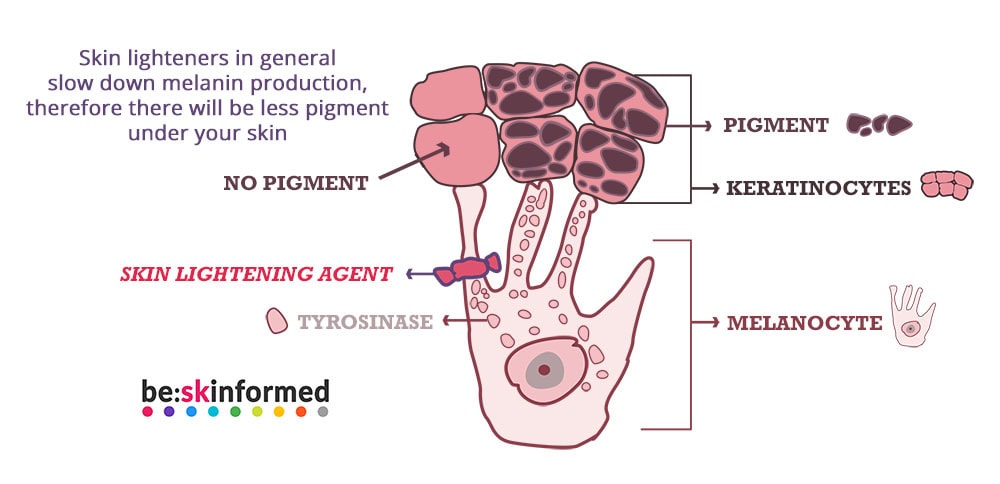
Once the diagnosis has been confirmed, management requires treatment with topical treatments or other procedures. These are meant to reduce the production of melanin on the area of application by interfering with various stages of melanogenesis.
The treatments are usually done hand in hand with other measures to address the underlying causes. Also, the stubborn and recurrent nature of melasma necessitates the need for long-term treatment.
Here are the various treatment options for melasma:
Hydroquinone
Hydroquinone is considered the gold standard for the treatment of melasma and other forms of hyperpigmentation. It effectively treats hyperpigmentation by inhibiting tyrosinase, the enzyme responsible for melanin formation and causing the complete necrosis of the melanocytes.
It comes in form of topical creams that can be bought OTC at 2% concentrations and at 4% with a prescription in most countries. However, there are concerns with its safety and controversy surrounding its use. As a result of this, many countries and regions have banned hydroquinone use in cosmetic products.
Azelaic Acid
Azelaic acid was initially used to treat acne. However, due to its ability to inhibit tyrosinase, it has been adopted as a treatment for various hyperpigmentary disorders, melasma included.
Compared to Hydroquinone, AzA is able to depigment discoloured skin at a comparable level and without the harmful effects of hydroquinone.
Retinoids
These are derivatives of Vitamin A. They were previously used in combination with hydroquinone but after being discovered to have their own effect on melanogenesis, they can now be used on their own.
They work by both reducing tyrosinase activity and speeding up the epidermal turnover. While using them on their own still works, better results have been reported when they are combined with HQ or corticosteroids.
Topical Steroids
These work by inhibiting melanogenesis. They are effective on their own but they are associated with skin hypopigmentation when used for a long time. Topical steroids are usually used in combination with other products such as HQ and retinoic acid.
Natural Skin Lightening Creams and Serums
These incorporate natural skin lightening ingredients that work by inhibiting melanin synthesis, increasing cell renewal, fighting radicals and exfoliating your skin to give rise to new cells. They do this effectively and without the dangers associated with other ingredients like Hydroquinone.
Natural skin lightening creams are used topically and have been proven to be safe and effective in getting rid of all forms of hyperpigmentation including melasma.
Related reading: Best Creams for Melasma
Procedures
If topical medications do not work, you might want to try procedures. Here are several that might just succeed:
Chemical Peels
During a chemical peel procedure, a chemical solution is applied on the skin with the intention of destroying the superficial layer of the skin in a controlled manner. When this is done, the skin exfoliates and peels off to reveal lighter, less blemished and evenly pigmented skin.
Some of the chemicals used include salicylic, trichloroacetic, glycolic and lactic acids. The strength of the solutions and the depth of the peels may depend on the severity of your condition, the target results and the type of your skin.
Lasers
The procedure makes use of concentrated beams of light to target and disrupt melanin granules in the upper dermis. The process also stimulates the growth of new cells which lead to a lighter skin tone.
There are different types of laser skin surgeries and your surgeon can help you choose the most suitable depending on your skin type, the condition of your skin, the results you are looking for, and your budget.
Dermabrasion
The procedure involves the use of a rotating device to remove the outer layers of the skin. This makes ways for a newer, smoother layer that is less blemished. Dermabrasion works better for fair skinned people as it causes more scarring or post-inflammatory hyperpigmentation on dark-skinned people. Microdermabrasion is less intensive and might work for mild or epidermal melasma for all skin types.
Tips for Preventing and Managing Melasma
Even if the exact causes of melasma remain unclear, we have established that several circumstances can increase your risk of getting melasma or aggravate an already existing condition. The following tips can help you either keep it at bay or stop it from becoming worse.
- Wear sunscreen daily regardless of the weather – since sunlight triggers melasma, choose a sunscreen that gives you broad-spectrum protection. A SPF of 30 or more should do.
- Beef-up your sun protection – sunscreen might not give you all the protection that you require. Enhance your protection by wearing wide-brimmed hats and sunglasses whenever you venture out. Avoid direct sun by sheltering in the shade whenever you can.
- Choose your skin care products wisely – Keep off products that might sting or burn your skin. These may cause post-inflammatory hyperpigmentation that can make the situation worse.
- Avoid waxing – this may cause inflammation that can worsen the situation. Look for other milder hair removal options.
Conclusion
Melasma is a skin condition that causes patches of hyperpigmented skin, usually on the face. Everybody can get melasma but pregnant women or those on hormonal birth control or hormone replacement therapy are at a higher risk. The darker skinned people and people with family history of melasma are also more likely to suffer. The situation can further be aggravated by exposure to sunlight.
Melasma is treated by addressing the underlying condition before using skin lightening products and procedures to address the discolouration. The treatments are usually long-term and should be used alongside measures to stop further aggravation of the situation. When proper procedure and treatments are adhered to, people with melasma can lead normal lives without having to deal with the emotional distress brought about by the condition.
About:
sonia knight
Sonia Knight is the founder of be:skinformed.
Apart from having her own experience with hyperpigmentation, Sonia has gained vast knowledge in the dermatology field. For more info on this, check out our about us page.




